How to Improve Egg Quality for Pregnancy
Egg quality is one of the most important factors in whether a woman is able to conceive, but it is a topic that many never think about until they are already struggling to get pregnant. Poor egg quality is caused by diminished ovarian reserve and is one of the most common causes of infertility, especially in women over 35.
Egg quality is important because it determines embryo quality. Poor egg quality is closely associated with chromosomal abnormalities in embryos, also known as aneuploidy.
In some cases, aneuploidy can cause birth defects, but more often it results in miscarriage, often at such an early stage that a woman does not even know she was pregnant.Problems with egg quality can mean that the resulting embryos don’t implant, or that the eggs fail to fertilize at all. Whether you are trying to conceive on your own or are getting ready to embark on IVF, how can you make sure your eggs are as healthy as possible?
1. Look at your lifestyle choices.
While there are currently no clinically proven ways to improve egg quality once it has begun to decline, researchers have been exploring how lifestyle choices may have a significant impact on reproductive health in general.There have not yet been any conclusive findings on what type of diet or exercise is best for egg quality specifically, but common sense and self-care will go a long way towards ensuring that your body as a whole is functioning at its peak potential for health. You are more than your eggs. You deserve to feel healthy for yourself and so that you’ll be ready to nurture a pregnancy when it comes. When you are trying to conceive it’s a good idea to start making choices “as if” you are already pregnant. Eat a balanced, healthy diet with plenty of protein, avoid foods known to be high in toxins, cut out nicotine, alcohol, and caffeine, and allow yourself time for regular, gentle exercise.
Being told “to relax” can be infuriating when you’re struggling with infertility, but reducing stress wherever you can actually does have health benefits. Stress triggers physiological reactions in the body which can cause a less-than-ideal environment for your eggs.
Don’t worry about avoiding all stress: it’s not possible and stressing out about stress is a vicious circle. But do give yourself tools for dealing with it when it arises. Meditation, relaxation techniques, and the support of friends, family, and professionals can really help you through the tough times.
2. Consider complementary therapies.
Nothing replaces a consultation with a qualified reproductive expert, but many women find that complementary, alternative therapies and treatments increase their sense of well being as they are trying to conceive. Fertility Massage, acupuncture and herbal medicine, as well as dietary supplements may all have a place in creating an optimal environment for your eggs.Just check with your doctor to be sure that there are no potentially harmful interactions between the herbs and supplements you’re taking any any prescribed medications. Don’t hesitate to go for an “egg checkup.”When a woman is born, her ovaries already contain a lifetime of eggs. Over the years, the number of these eggs is whittled down, and egg quality begins to decline, usually in her early thirties.This decline accelerates through the late thirties and early forties, and continues until she finally reaches the end of her fertile years.Early and regular monitoring of your egg quality and quantity is important.Waiting until you are already having trouble may mean losing precious time. Going to a fertility clinic for these tests is a relatively low-cost and low-commitment way to get an accurate snapshot of your fertility at a given point in time, and it can help you make decisions as you move forward.
TESTS
1. Antral Follicle Count (ultrasound). Antral follicles are small ovarian follicles which can be seen (and counted) through an ultrasound. By counting the number of visible antral follicles, a doctor can predict how many primordial follicles (which are microscopic, each containing an immature egg) a woman is likely to have. More follicles means a higher ovarian reserve.
2: Day 3 FSH (blood test). Follicle stimulating hormone, or FHS, is one of the most important hormones in ovulation. It is produced by the pituitary gland and stimulates the follicles in your ovaries to mature and release an egg when you ovulate.[1:08 PM, 5/14/2019] Fertility support group: Measuring FSH levels early in the menstrual cycle allows doctors to see how hard your body is working to make ovulation happen. Your body will keep making more and more FHS until you ovulate: if you don’t ovulate at all, your pituitary gland
Take 4 Tablespoons Of This Every Morning And Say Goodbye To Clogged Arteries, High Blood Pressure, And Bad Cholesterol!
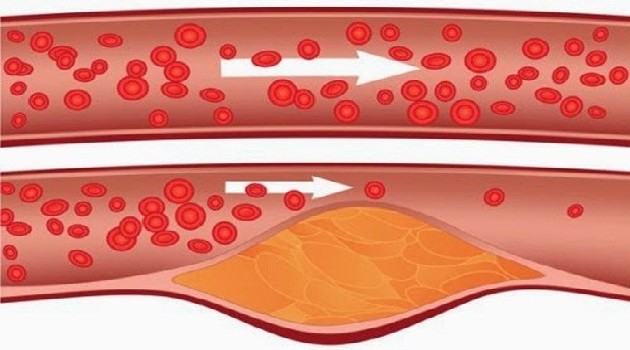
The regular consumption of this powerful drink will help you to unclog your arteries, treat the bad cholesterol, and reduce high blood pressure.
Today, numerous people suffer from high cholesterol levels. The most common reasons are the fast lifestyles, stress, and improper care for our health. If your cholesterol is more than 4,60 to 6,20 mmol/L, then you might experience some serious health issues.
Here is the amazing recipe, which will unclog your arteries and reduce your high blood pressure:
Ingredients:
- 1 kg lemons
- 12 cups of water
- 3 tablespoons of baking soda
- 5 or 6 bunches of parsley
Preparation:
At first, you should wash the lemons in a cold water. Then, in a warm water add the already chopped lemons and put 1 bag of baking soda. Let it sit for an hour.
Chop the parsley and add it into the mixture, then cook it for another 2-3 hours on low heat. Once your drink is ready, put it into a glass container and keep it in the fridge.
Drink 4 tablespoons of the syrup every morning on an empty stomach. With this amount, you should be sufficient for a twenty-day administration.
The treatment will provide amazing benefits for your health, therefore do not hesitate to try it!
Vaginal Yeast Infection
Vaginal Yeast Infection
Symptoms
Causes
Diagnosis
Treatment
Alternative remedies
Prevention
What is a vaginal yeast infection?
A vaginal yeast infection, also known as candidiasis, is a common condition. A healthy vagina contains bacteria and some yeast cells. But when the balance of bacteria and yeast changes, the yeast cells can multiply. This causes intense itching, swelling, and irritation.
Treating a vaginal yeast infection can relieve symptoms within a few days. In more severe cases, it may take up to two weeks.
Vaginal yeast infections aren’t considered a sexually transmitted infection (STI). Sexual contact can spread it, but women who aren’t sexually active can also get them. Once you get a yeast infection, you’re also more likely to get another one.
What are the symptoms of a vaginal yeast infection?
Vaginal yeast infections have a common set of symptoms, such as:
vaginal itching
swelling around the vagina
burning during urination or sex
pain during sex
soreness
redness
rash
Whitish-gray and clumpy vaginal discharge is another telltale symptom. Some people say this discharge looks like cottage cheese. Sometimes the discharge may also be watery.
Usually the length of time your yeast infection is left untreated has a direct impact on how severe your symptoms may become.
What causes vaginal yeast infections?
The fungus Candida is a naturally occurring microorganism in the vaginal area. Lactobacillus bacteria keeps its growth in check.
But if there’s an imbalance in your system, these bacteria won’t work effectively. This leads to an overgrowth of yeast, which causes the symptoms of vaginal yeast infections.
Several factors can cause a yeast infection, including:
antibiotics (they decrease the amount of Lactobacillus [“good bacteria”] in the vagina)
pregnancy
uncontrolled diabetes
weak immune system
poor eating habits, including a lot of sugary foods
hormonal imbalance near your menstrual cycle
stress
lack of sleep
A specific kind of yeast called Candida albicans causes most yeast infections. These yeast infections are easily treatable.
If you’re having recurring yeast infections or problems getting rid of a yeast infection with conventional treatment, then a different version of Candida might be the cause. A lab test can identify what type of Candida you have.
How are vaginal yeast infections diagnosed?
Yeast infections are simple to diagnose. Your doctor will ask about your medical history. This includes whether you’ve had yeast infections before. They may also ask if you’ve ever had an STI.
The next step is a pelvic exam. Your doctor will examine your vaginal walls and cervix. They’ll also look at the surrounding area for external signs of infection.
Depending on what your doctor sees, the next step may be to collect some cells from your vagina. These cells go to a lab for examination. Lab tests are usually ordered for women who have yeast infections on a regular basis or for infections that won’t go away.
How is a vaginal yeast infection treated?
Each yeast infection is different, so your doctor will suggest a treatment that’s best for you. Treatments are generally determined based on the severity of your symptoms.
Simple infections
For simple yeast infections, your doctor will usually prescribe a one-to-three–day regimen of an antifungal cream, ointment, tablet, or suppository. These medications can be in either a prescription or and over-the-counter (OTC) form.
Common medications include:
butoconazole (Gynazole)
clotrimazole (Lotrimin)
miconazole (Monistat)
terconazole (Terazol)
fluconazole (Diflucan)
Women with simple yeast infections should follow up with their doctors to make sure the medicine has worked.
You’ll also need a follow-up visit if your symptoms return within two months.
If you recognize that you have a yeast infection, you can also treat yourself at home with OTC products.
Complicated infections
Your doctor will more than likely treat your yeast infection as if it were a severe or complicated case, if you:
have severe redness, swelling, and itching that leads to sores or tears in your vaginal tissue
have had more than four yeast infections in a year
have an infection caused by Candida other than Candida albicans
are pregnant
have uncontrolled diabetes or a weak immune system from medication
are HIV-positive
Possible treatments for severe or complicated yeast infections include:
14-day cream, ointment, tablet, or suppository vaginal treatment
two or three doses of fluconazole (Diflucan) and immune booster
long-term prescription of fluconazole (Diflucan) taken once a week for six weeks or long-term use of a topical antifungal medication
If your infection is recurring, you may also want to see if your sexual partner has a yeast infection. Remember to use condoms when having sex if you suspect either of you has a yeast infection.
What natural and alternative treatments are available?
You can try to treat vaginal yeast infections with natural remedies if you’d like to avoid taking prescription medication, but these aren’t as effective or reliable as the indicated medications. Some popular natural remedies include:
coconut oil
tea tree oil cream
garlic
boric acid vaginal suppositories
plain yogurt taken orally or inserted into the vagina
Always make sure your hands are clean before applying creams or oils to your vagina.
You may also want to talk to a doctor before trying natural remedies. This is important because:
If your symptoms are due to something other than a simple yeast infection, your doctor can help diagnose your condition.
Some herbs can interact with medications you may be taking or can cause other unintended side effects.
How do you prevent vaginal yeast infections?
Take up
eating a well-balanced diet
eating yogurt or taking supplements with lactobacillus
wearing natural fibers such as cotton, linen, or silk
washing underwear in hot water
replacing feminine products frequently
Avoid
wearing tight pants, pantyhose, tights, or leggings
using feminine deodorant or scented tampons or pads
sitting around in wet clothing, especially bathing suits
sitting in hot tubs or taking frequent hot baths
douching
Often you probably know exactly what led to your yeast infection.
For example, some women experience these infections every time they take antibiotics.
By recognizing your own risk factors, you can prevent future infections.
Decidual bleeding or period?
QUESTION – Decidual bleedingor period?
I had unprotected relations with my boyfriend in the middle of my menstrual cycle and I was expecting my next Menstrual Period on 23 February. But I had very unusual “period” on 25 February – it was short and light. My friends told me it could be so called “decidual bleeding” and they advice me to buy a Pregnancy test How to check if it is my regular period or decidual bleeding?
ANSWER

DECIDUAL BLEEDING or PERIOD?
Many women can experience episodes of bleeding during first trimester of pregnancy – bleeding could be brown or red, light and short. Some women (mothers and grandmothers) tell about periods during first 1-2 months of pregnancy. But in reality it is not normal menstrual period but it is so called “decidual bleeding”.
“Decidual bleeding” is the name for specific bleeding during pregnancy that may occur around the time that a pregnant woman would otherwise expect her menstrual period. The phenomenon is fairly rare (20-35%) and usually does not last longer than the first few months of pregnancy – this bleeding can be similar to a menstrual period and can occasionally prevent women from realizing that they are pregnant until other signs develop.
During pregnancy the whole women health is changed dramatically and most women could recognize changes very early (even before the day of expected menstrual period).

Decidual bleeding
What is difference between decidual bleeding and regular menstrual period?
Actually decidual bleeding is “period-like” bleeding during pregnancy – though this bleeding may resemble menstruation, it actually is something different altogether.
What is period/menstruation? Normal regular menstrual period is an essential part of women health. During menstrual cycle women produce several hormones in very specific rhythm and these hormones signals to all reproductive organs – signals to follow biological menstrual rhythm to perform certain body biological actions. From the beginning of the menstrual cycle hormones are increasing and causing ovaries to release an egg that travels from ovary through Fallopian tubes. Meanwhile, a protective layer of blood and tissue thickens along the walls of the uterus. If the egg is not fertilized (absence of pregnancy), hormone levels will drop, signaling body that it is the time to shed the lining that built up in uterus. This is what causes menstruation (so called “period”).
During pregnancy hormone production is changed dramatically – all female body hormones and organs (especially reproductive organs) are completely focused on providing support for baby. The brain sends signals to ovaries to stop the menstrual cycle in order to insure proper environment for baby healthy development – as a result, instead of dropping, female hormones continue to rise for the next nine months. This helps the uterus prepare for the growth and nourishment of the baby.
Sometimes during pregnancy women hormones can get out of whack, causing you to lose parts of the lining of your uterus – this is actually the decidual bleeding. This is especially common in the early stages of pregnancy, before the lining has completely attached to the placenta.
Cottage cheese discharge
Vaginal discharge is the normal way how body keeps itself clean and hygienic. According to the type of vaginal discharge you even can guess about your fertility cycle. Every woman has normal vaginal discharge with specific texture, color and personal smell. If you notice changes in your vaginal discharge, it could mean changes in your vaginal microflora. Often women could experience cottage cheese discharge. According to health experts, white cottage cheese discharge (thick, white, curdy discharge) from the vagina is the typical symptom of vaginal yeast infection (vaginal candidiasis) – actually it is vaginitis triggered by Candida albicans. Over 75% of all women will get vaginal yeast infection at some point in their lives. So, while unpleasant, yeast infection is really quite common.
Cottage cheese discharge is not the only symptom of vaginal yeast infection. In most cases women suffer also from other symptoms such as: Vaginal itching (mild to intense);
Vaginal soreness, irritation or burning sensation (especially during intercourse);
Redness around the vagina.
Sometimes vaginal yeast infection can be combined with other sexually transmitted diseases such as chlamydia , Trichomoniasis , or Gonorrhea and some other infections.
Symptoms of combined infections could be more severe including different types of vaginal discharge (green vaginal discharge, grayish discharge or yellow discharge), pelvic pain or abdominal pain, vaginal smell (fishy vaginal smell, foul-smelling) and fever.
Cottage cheese discharge – yeast infection – causes
Cottage cheese discharge
Vaginal yeast infection arises when suddenly appeared the bacterial imbalance in the vagina which causes yeast Candida over-population.
Main vaginal yeast infection causes include the following:
- Antibiotics – antibiotics can kill some vaginal bacteria and it can trigger overgrowth of Candida (yeast infection);
- Diabetes – during diabetes the vagina could experience increased levels of sugar, allowing yeast to grow more rapidly;
- Weakened immune system – triggered by stress, infections or other diseases;
- Vaginal hygiene – vaginal deodorants, perfumed soaps, bubble baths or douching may cause vaginal irritation and upset the normal balance;
- Menstruation decreased hormone levels could change vaginal environment which may contribute to yeast infections;
- Pregnancy – many pregnant women experience vaginal yeast infection triggered by dramatic hormonal changes;
- Clothing – tight jeans, wet bathing suits, nylon underwear and synthetic swimsuits can retain heat and moisture, creating an environment that encourages the growth of yeast.
Cottage cheese discharge – diagnosis
Vaginal yeast infection with cottage cheese discharge combined with vaginal itching could be pretty disturbing and unpleasant. First advice would be to visit your gynecologist for proper diagnosis and adequate treatments. But is you need to check it yourself and find cheap solutions, you can start with home diagnostic tests which will identify your vaginal infection clearly.
Once you confirm that your cottage cheese vaginal discharge is actually the symptom of vaginal yeast infection, you can use one of recommended “Yeast infection home remedies”.
Home Remedies :
Over-the-counter treatments. Anti fungal treatments in the form of creams or pessaries can be purchased over the counter to treat yeast infections. …
Boric acid. Vaginal boric acid capsules can work for women with a yeast infection. …
Tea tree oil. Adding diluted tea tree oil to a tampon and inserting this into the vagina overnight.
Probiotic supplements. …….
Natural yogurt. …
Bikini Bumps
The perfect bikini zone is a vital part of embracing swimsuit season. Bikini line is the most sensitive area for shaving and irritated bikini zone as well as most scary bikini bumps can be a problem. Usually bikini bumps appear when the hair follicles are twisted and pulled due to a razor blade. Shaving could lead to the development of bikini bumps or ingrown hairs. Usually bumps appear when hair follicles get infected by bacteria – it causes inflammation, redness and pain in affected area.
There are several recommendations and techniques that every woman should absolutely keep in mind before, during and after shaving bikini zone. Just remember that prevention is always better and easier than treatment.
Bikini bumps – prevention recommendations
Don’t shave bikini line every day
It is better to let hair grow out a bit and old bumps to heal before shaving. The best is to shave your bikini zone under the warm shower and preferably rinse off with cold water. It is well known that warm water can soften hair and make sensitive skin less prone to irritation. At the same time, rinsing with cold water will close up skin pores which will prevent infections, inflammation and irritation.
Bikini bumps – treatment

Bikini bumps
Creams
Several creams can be effective including antibacterial creams, antibiotic creams, Retin-A cream, hydrocortisone cream. Local application of mentioned creams can reduce swelling and redness caused by inflammation.
Aspirin
Crushed aspirin paste can support healing of irritated bikini line bumps due to exfoliation, liberation of pores and release of trapped ingrown hairs. At the same time, aspirin can kill some bacteria responsible for redness and inflammation.
Aloe
Aloe Vera lotion or gel can heal irritated bumps due to its
anti-bacterial and anti-inflammatory properties. Local application on
affected area will help you to rid of bumps.
Tea tree oil
Tea tree oil has magic natural antiseptic and antibacterial properties which can not only treat but also prevent bumps on Bikini Mixture of tea tree oil with water should be applied with cotton pads.
Apple Cider Vinegar
Apple Cider Vinegar can restore bikini skin’s pH levels and help promoting healing as well as preventing any blistering. Apple Cider Vinegar should be always diluted before applying on the skin.
Black tea
Black tea has anti-inflammatory property and it can calm redness and
irritation. Just apply cold black tea tissue on bikini line. Some
experts recommend black tea ice cubes to be applied just after shaving.
Neosporin
Neosporin local application soon after shaving can eliminate bumps on
bikini line. This medication can be used easily after each shaving –
keeping your bikini line bump-free.



